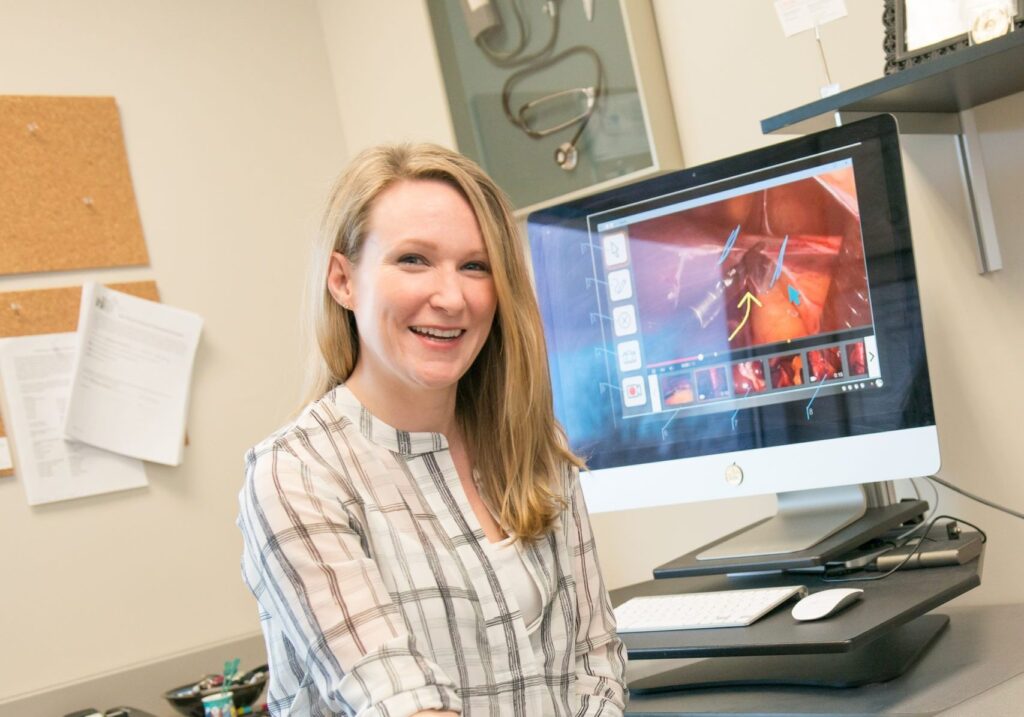
After years of gradual expansion, telemedicine has grown dramatically during the COVID-19 pandemic, allowing patients to consult with medical professionals from a distance, without traveling to an office or hospital. But the availability of telemedicine has not yet risen to meet demand, says UMBC’s Helena Mentis, associate professor of information systems (IS).
New strategies are needed to scale-up telemedicine, and more entry-level medical professionals require training on how to provide care to patients virtually. Such training is particularly challenging when clinicians sharing their knowledge are in different locations than the people being trained. A UMBC team is taking on these challenges.
UMBC researchers have received a nearly $150,000 planning grant from the National Science Foundation (NSF) to study how telemedicine can be scaled more effectively, including meeting the complex training needs of medical professionals. Mentis, who is also an associate dean in the College of Engineering and Information Technology, is the principal investigator (PI) on the grant. She will work with Andrea Kleinsmith, assistant professor of IS; Anita Komlodi, associate professor of IS; Gary Williams, clinical coordinator in emergency health services; and Christine Yee, former assistant professor of economics, now an economist at Boston University and the Partnered Evidence-based Policy Resource Center, who are all co-PIs.

Mentis explains that this grant is an extension of her work on surgical telemedicine, which was the focus of her NSF CAREER award in 2016. “Whereas my prior work was on one physician communicating with one physician, this grant is looking at how we can scale the benefits of telemedicine with a hub and spoke model,” she says.
Addressing big ideas
The grant is part of NSF’s Big Ideas initiative, which focuses on “ten bold, long-term research and process ideas that identify areas for future investment at the frontiers of science and engineering.” Mentis explains that this research is specifically related to the Future of Work at the Human-Technology Frontier.
The research team will begin building a framework to better understand telemedicine through three approaches. First, they will develop and host a workshop for emergency healthcare leaders and educators, people who develop telemedicine systems, and health economists to discuss existing telemedicine challenges and identify possible innovative solutions.

Second, they will complete an exploratory study to assess the cognitive, communicative, and affective loads experienced by telemedicine professionals in the field and by seasoned clinicians as they lead telemedicine training. Interviews with emergency medical services (EMS) professionals from the greater Baltimore region will provide data for this component.
The final element of this work will be for the research team to connect with community partners to understand the challenges of telemedicine-at-scale. They will also examine how expanding telemedicine could impact the EMS workforce and healthcare costs
Yee explains that through the grant, there will be interviews conducted with EMS managers to find out how they identified and hired their current workforce. “We hope to learn about the expenses related to the current practice of off-site emergency services and transportation to hospitals and other medical institutions,” she says. “We also will be interviewing current and potential EMTs and paramedics about their considerations regarding the EMS career path, including training, burnout, compensation, and risks.”
Developing scalable solutions
The researchers will interview EMS professionals in greater Baltimore to learn about the challenges they face when providing care through telemedicine. They will also examine how telemedicine might offer an entry-level pathway for high school graduates who are interested in pursuing a healthcare career.

Williams explains that in early 2019, EMS 2050 was released. This guide informs EMS leaders and educators about the future of the field, and one of the guiding principles is a focus on being adaptable and innovative. “The document speaks specifically about telemedicine and EMS and how we improve patient care by bringing this technology to the forefront,” he says. “The timing is perfect with receiving this grant and the release of EMS 2050. We need this type of research to start making changes and finding new ways to provide patient care to everyone, no matter where they live.”
The existing EMS infrastructure and educational pathways explored through this process will inform the team’s recommendations for scaling telemedicine. By finding new ways to meet high demand for telemedicine services, the team hopes to relieve some of the strain on emergency medical technicians and other healthcare providers who are stretched beyond capacity.
“We began this work with the intention to impact healthcare in the far off future, but as we have seen in the past 6 months, that future is here now,” says Mentis. “Equitable, scalable, and affordable healthcare are of paramount importance and this grant is a huge step in working with our healthcare partners to identify sustainable change.”
Banner image: Telemedicine consultation equipment. Photo by Sergio Santos, used under CC 2.0.