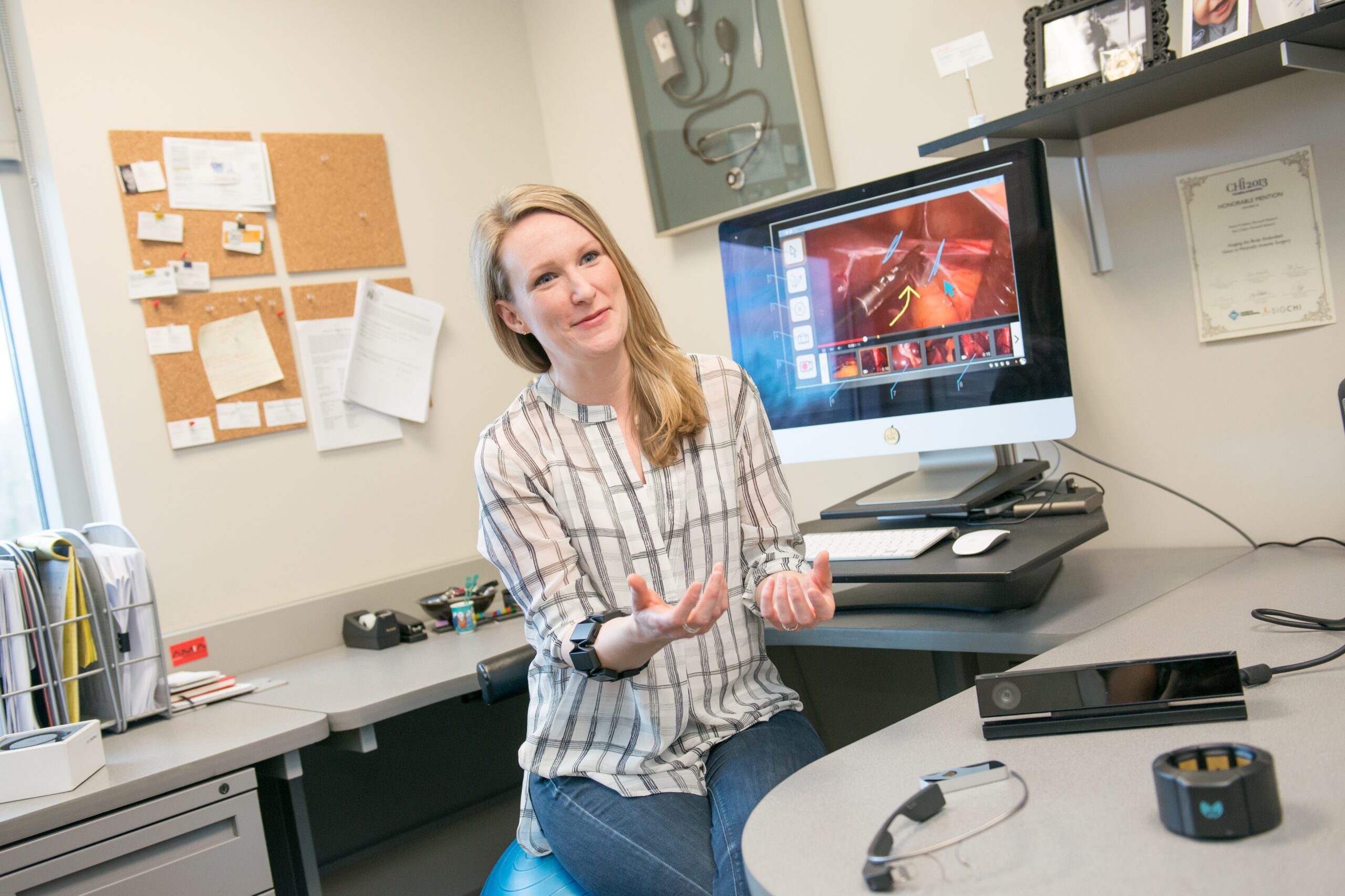
Helena Mentis, assistant professor of information systems and 2016 recipient of a prestigious NSF CAREER Award, is seeing results in new research using activity trackers and other motion sensors to assess movement and inform treatment for patients with Parkinson’s disease, based in the finding that daily walking has been shown to benefit such patients.
Mentis, Lisa M. Shulman, director of the University of Maryland Parkinson Disease and Movement Disorders Center, and their collaborators have recently shared their findings through articles in notable research publications as well as presentations at the Conference of Human Factors in Computing Systems in Denver, CO.
In “Co-Interpreting Movement with Sensors and Assessing Parkinson’s Patients’ Deep Brain Stimulation Programming,” published in Human-Computing Interaction, Mentis, Shulman and their co-authors explain how they designed and developed a sensor using Leap Motion devices to track and assess the movement of patients with Parkinson’s disease during Deep Brain Stimulation. They noted the movement in their upper limbs during follow-up appointments. They found that the sensors can help assess movement, but sometimes the sensors can interfere with how physicians assess movement by the patient. Mentis and her collaborators found that the way the sensor data is presented can impact how the data is interpreted and used to make decisions regarding treatment.
Mentis presented a paper “Crafting a View of Self-Tracking Data in the Clinical Visit” at the Association for Computing Machinery Special Interest Group on Computer-Human Interaction Conference on Human Factors in Computing Systems (CHI 2017). The paper, published by the Association for Computing Machinery, details what happened when Mentis and her collaborators provided Fitbit activity trackers to Parkinson’s patients for a month prior to a follow-up meeting with a neurologist. The study found that the Fitbit provided clear activity data and easy to read charts that could inform patient-physician conversations during follow-up visits, leading to an active shared decision-making process about the role of exercise in treatment plans. Anita Komlodi, associate professor of information systems, Shulman and other collaborators co-authored the paper.
Image: Helena Mentis. Photo by Marlayna Demond ’11 for UMBC.